Health Strategy.
Breast cancer cannot be considered a single disease due to the fact that it is characterized by different pathological and molecular subtypes, which are treated by different methods and have different clinical outcomes.
Currently, there are about 20 subtypes of breast cancer. To classify it, various characteristics are used: degree of development; degree of aggressiveness; place of onset of the disease (milk ducts, lobules); developmental features; molecular markers inherent in the tumor; as well as other factors.
A tumor that originates from epithelial cells (cells that line the surface of the glands and vessels of the mammary gland) is called a carcinoma, and a tumor that develops from connective tissue is called a sarcoma.
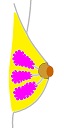
The mammary gland is located on the pectoralis major muscle, extending from the collarbone to the armpit and sternum. A healthy breast contains connective tissue, lobules, ducts, adipose tissue, nerves, blood and lymph vessels.
Connective tissue, forming strips of ligaments, runs from the skin to the muscles, thereby supporting the breast.
The lobules are groups of glands that produce milk. Each breast contains 15 to 28 lobules, each of which is in turn made up of several small sections called lobules. The process of milk production is stimulated by hormones under the influence of pregnancy and childbirth of a woman.
The ducts are the vessels through which the milk produced by the lobules flows from the lobules to the nipple. The number of ducts generally does not match the number of lobules because many ducts have several common openings on the surface of the nipple. The width of the ducts under the skin is very thin, but gradually increases deep into the nipple, having points of constriction and expansion *.
The nipples are the convex part in the center of the areola with holes for the source of milk.
The fatty layer fills the space between the lobes and ducts.
Areola is a brownish round area around the nipple that secretes small amounts of oily lubricant to coat the nipple and areola.

The tissue around the lobules and ducts is called the stroma. Inside the stroma, blood vessels deliver oxygen, glucose and other substances necessary for the normal functioning of cells. The lymph vessels are filled with a clear fluid called lymph. Lymph transports immune cells, water and nutrients to breast tissue and drains to nearby lymph nodes carrying toxic waste.
Breast tumors are most commonly diagnosed in spring and autumn *, and most often they develop in the upper outer quarter of the breast (closest to the armpit) * because that part of the breast contains more glandular tissue. The epithelial tissues of the ducts and lobules are predominantly affected, thus forming a carcinoma, on which our main attention will be focused.
Cancer is an extreme case of pathology, occupying an insignificant place in the total number of breast diseases. Non-cancerous painful conditions of the breast are much more common. Some of them can cause cancer-like symptoms.
The most common benign or non-tumor disease states of the breast are: calcifications, cysts, fibrosis, fibroadenoma, intraductal papilloma, adenosis, lipomas and some others *. High radiographic density of breast tissue is not considered a disease, however, an increase in tissue fibrosis can contribute to the appearance and development of cancer * *.
A disease such as hyperplasia, in which breast epithelial cells divide too frequently, is the first step towards a tumor. Women with atypical hyperplasia have an increased risk of developing breast cancer *.
There are nodular and diffuse types of malignant tumors.
Nodular tumor. This is the most common type of cancer, which is the formation of nodules - affected areas of tissue. They can be felt on palpation, noticed by a change in skin tone (yellowish, reddish, brownish), as well as by possible roughening of the skin and discharge from the nipple.
Diffuse tumor. This is a rarer, but more dangerous type of cancer that develops rapidly, gives early metastases and has a poor prognosis. Diffuse cancer is characterized by swelling of the skin and gland tissue; redness and hyperthermia of the skin; and significant local distribution.
Diffuse cancer has its subspecies:
• infiltrative, in which a dense painless or slightly painful formation is formed. At the same time, the mammary gland increases in size and swells, and the skin itself acquires a characteristic «orange peel» appearance.
• inflammatory, in which painful seals form inside the breast, and the breast itself swells and becomes bluish.
• armored, in which the breast is pigmented, wrinkled and reduced in volume, and multiple nodules appear, which then merge into one large tumor.
• intraductal, difficult to detect in the initial stage, when the only symptom is bloody discharge from the nipple.
• certain other types of cancer.
In the tissues of the mammary gland in the ducts and lobules, 2 layers of cells are distinguished: luminal - facing the lumen of the duct, and basal - adjacent to the basement membrane. Depending on which of these cells was the ancestor of cancer, the type of malignant breast tumor is determined - respectively, luminal and basal.
According to the degree of invasiveness, invasive and non-invasive cancers are distinguished.
Non-invasive cancer (in situ) is located in a certain place and does not spread to the surrounding tissues, lobules or ducts of the gland.
Invasive cancer is able to expand, invade nearby stromal tissue in the breast, and then spread to distant sites such as the bones, lungs, liver, or brain, forming secondary tumors (metastases).
Normal cells in the process of differentiation acquire specific phenotypic forms that reflect their function as part of the mammary gland system. When cell division becomes uncontrolled, cell differentiation is lost.
The degree of differentiation does not assess the level of development of the tumor, but how the cancer cells look under the microscope and how quickly they are able to grow and spread. In general, a lower grade corresponds to a slower growing tumor, and a higher grade corresponds to a faster growing tumor.
To assess the prospects for tumor development, the following levels are used:
Grade I (well differentiated) - cancer cells resemble normal cells in appearance and do not grow rapidly;
II degree (moderate differentiation) - cancer cells bear little resemblance to normal cells and grow faster than normal ones;
Grade III (poorly differentiated) - Cancer cells look abnormal and may grow or spread more aggressively.
An increase in signs of loss of differentiation by mammary gland cells indicates the progression of the disease and a worsening prognosis *.
Genomic studies allow for a more specific systematization of breast cancer based on genes and proteins. Although it is not capable of classifying all varieties of human breast cancer, for simplicity they are grouped into one of three categories based on the type of receptor present or absent on tumor cells: estrogen receptor (ER+/ER–), progesterone receptor (PR+/PR–) and human epidermal growth factor receptor type 2 (HER2+/HER2–). Recent studies have found that there are other receptors that may be therapeutic targets in breast cancer, such as the androgen receptor (AR), vitamin D receptor (VDR) and aryl hydrocarbon receptor (AHR).
These clinically significant breast cancer phenotypes are now recognized (listed in order of decreasing cancer cell differentiation and worsening prognosis *).
Luminal subtype A (ER+ and/or PR+, HER2–, Ki67 < 14%), estrogen-dependent low-aggressive tumors, occur in 56-61% of cases. This is the most common subtype for every race and age. These tumors usually grow slowly. Treatment often includes hormone therapy.
Luminal subtype B (ER+ and/or PR+, HER2+ or Ki67 > 14%), estrogen-dependent aggressive tumors, occur in 9-16% of cases. These tumors tend to grow faster than luminal subtype A tumors. Subtype B, compared to subtype A, shows increased recurrence and reduced disease-free survival * with much lower 5- and 10-year survival rates * *, and worse response to any existing therapies *. Chemotherapy and hormone therapy targeting the HER2 receptor can be used to treat this subtype.
Luminal HER2 subtype (ER+ and/or PR+, НЕR2+). Similar to the luminal subtype B.
HER2-positive subtype (ER–, PR–, HER2+), estrogen-independent aggressive tumors; occur in 8-16% of cases. Depending on the stage of the cancer, treatment options for HER2 positive breast cancer may include a combination of surgery, radiation, chemotherapy, and/or targeted therapy. HER2+ cancer cells respond to treatment with immune monoclonal antibodies (such as trastuzumab). Unfortunately, approximately 75% of patients with HER2 tumor expression do not respond to trastuzumab, and approximately 15% of those who respond to treatment eventually develop metastases *. Tumors of the HER2 subtype often metastasize to the brain *, avoiding further inhibition by HER2-targeting antibodies, which are difficult to cross the blood-brain barrier due to their large molecular size.
Triple Negative Breast Cancer (TNBC) is subdivided into basaloid (ER–, PR– и HER2–, cytokeratin 5/6+ and/or HER1+), accounting for 75-80% of TNBC cases, and non-basaloid (ER–, PR– и HER2–, cytokeratin 5/6– and/or HER1–), accounting for 20-25% of TNBC cases. These are estrogen-independent, highly aggressive tumors; and occur in 8-20% of all cases of breast cancer, often in women using hormonal contraceptives. Women who inherit a BRCA1 germline mutation carry a 60-80% risk of developing breast tumors * *, more than 80% of which are triple negative subtypes *. This subtype of breast cancer is usually highly invasive and most commonly begins in the thoracic ducts.
Because the malignant cells of this subtype of cancer do not contain estrogen, progesterone, or HER2 receptors, they will not respond to hormone therapies or drugs that work by blocking these proteins. Therefore, in triple-negative cancer, conventional means are used: radiation, complex chemotherapy and non-HER2-targeted therapy, which often do not slow down the development of the tumor *. The clinical response is approximately 40-45% *. After chemotherapy followed by surgical removal of the tumor, 12-28% of patients with TNBC achieve a complete response and have a good prognosis * *. However, patients with TNBC have a significantly lower overall survival than those with other subtypes *.
In fact, TNBC has several varieties, which will be discussed in the Specific Therapy section†. Many TNBC cells are AR positive, allowing androgen inhibitor therapy to be used against them; the rest of the TNBCs are AR-negative, and have the code name Quadriple Negative Breast Bancer (QNBC).
A particularly severe case of TNBC is Inflammatory Breast Cancer (IBC). It is the most aggressive TNBC and is characterized by rapid development, resistance to chemotherapy, and early metastases. Although the inflammatory type accounts for only 2-5% of all breast cancers, it shows a poor prognosis with a 40% five-year survival compared to 87% for all breast cancers.
Cancer subtype is associated with median survival and with the pattern of metastasis. Ten-year patient survival rates are: 70% (luminal A), 54.4% (luminal B), 46.1% (luminal HER2+), 48.1% (HER2+), 52.6% (basaloid triple negative), and 62. 6% (non-basaloid triple negative). The median survival in years of patients with distant metastases is: 2.2 years (luminal A), 1.6 years (luminal B), 1.3 years (luminal HER2+), 0.7 years (HER2+) and 0.5 years (basaloid triple negative) *.
Breast cancer most commonly metastasizes to the bones (70.6%), liver (54.5%), and lungs (31.4%), and HER2+ tumors affect the brain more frequently than HER2– *. Approximately 40% of women with HER2+ get brain metastasis. ER– subtypes are characterized by earlier metastasis. The percentage of recurrence after organ-preserving surgery for the HER2 subtype is 10%, for the triple negative subtype - 6.1%, and for the luminal subtype A - 4.7%. The vast majority of relapses occur within the first 5 years, but they can occur up to 15 years after completion of therapy.
The state of the molecular subtype and tumor receptor can, in many cases, change as the disease progresses, developing resistance to the respective targeted therapies. Thus, 21% of recurrent tumors have changes in the previous state of ER/PR or HER2 * receptors. Thus, the status of the markers should be checked each time before a treatment plan is drawn up, since treatment options considered effective in the primary stage of cancer may not be optimal in later stages, including relapses and metastases. This is especially important given that up to 20% of ER and PR immunohistology scores can be false negatives or false positives *. Moreover, the tumor may contain several different child mutated clones, which further confuses the picture.
To address these issues, testing of fluid biopsies (as circulating tumor cells or circulating free DNA) has been proposed in recent years as a tool to understand disease heterogeneity and the changes that occur during tumor development * *.
Further in the text, there will be different breast cancer cell lines that are most often used in laboratory studies * *, the differences between which are summarized in the following table.
Cell line |
Classification |
ER |
PR |
HER2 |
Mut. р53 |
Type |
MCF-7 |
Luminal subtype A |
+ |
+ |
- |
- |
Invasive ductal carcinoma |
BT474 |
Luminal subtype B |
+ |
+ |
+ |
+ |
Invasive ductal carcinoma |
MDA-MB-453, SKBR3 |
Luminal subtype |
- |
- |
+ |
+ |
Adenocarcinoma |
HCC1569 |
Basaloid subtype A |
- |
- |
+/- |
+ |
Metastatic carcinoma |
MDA-MB-231, MDA-MB-468 |
Basaloid subtype B |
- |
- |
- |
+ |
Adenocarcinoma |
SUM190 |
Non-basaloid subtype |
- |
- |
+ |
+ |
Inflammatory cancer |
The accepted classification of subtypes of breast tumors is too simplistic, as it is limited exclusively to cancerous cells. However, the tumor consists not only of cancer cells, but also of many others - normal epithelial, immune, migrating cells, etc., which also differ in a variety of phenotypes or dysfunctions. Thus, the combination of these differences determines the individuality of each tumor, and knowledge of these features allows for more personalized treatment *.
Breast cancer is also classified by the place of origin of the disease - in the lobules or in the ducts.
Some of the more common types of breast cancer and some of their subtypes are listed below.
Ductal carcinoma. The most common type of cancer that affects the breast ducts that carry milk from the lobules to the nipple.

Non-invasive ductal carcinomas are divided into several subtypes, mainly depending on the appearance of the tumor: micropapillary, papillary, solid, ethmoid, and comedo. The chance of recurrence after surgery is less than 30%, most of which occur 5-10 years after the initial diagnosis. Adding radiation therapy to a sparing operation reduces the risk of recurrence by half. Currently, the long-term survival of patients with non-invasive ductal carcinoma is approaching 100%.
Invasive ductal carcinoma begins in the milk ducts and spreads to nearby breast tissue. It accounts for more than 70% of invasive forms of breast cancer. The 10-year survival rate is 35-80% *. For patients with ductal carcinoma, surgical removal of the tumor and diseased tissue, and long-term systemic treatment with tamoxifen, are recommended to prevent recurrence.
There are rarer subtypes of invasive ductal carcinoma:
Medullary ductal carcinoma accounts for 3-5% of breast cancer cases and affects mainly women closer to 50 years old, and more often women with a BRCA1 gene mutation. These carcinomas are less likely to involve the lymph nodes, are more responsive to treatment, and may have a better prognosis than most other common subtypes of invasive ductal carcinoma. The 10-year survival rate is 50-90%. At the same time, such tumors are often triple negative. For the treatment of medullary ductal carcinoma, surgery is practiced, first of all, as well as chemotherapy and radiation therapy.
Mucinous ductal carcinoma accounts for less than 2% of breast cancers and mainly affects postmenopausal women. Cancer cells of such a tumor are surrounded by mucus and are usually positive for estrogen and/or progesterone receptors and negative for the HER2 receptor. The 10-year survival rate is 80-100%. Surgery is usually recommended for the treatment of mucinous ductal carcinoma, as well as some adjunctive therapies such as radiation, hormonal therapy, and chemotherapy.
Papillary ductal carcinoma accounts for less than 1% of invasive types of breast cancer and affects, in most cases, postmenopausal women. Outwardly, it manifests itself in the form of fern-like formations of cancer cells. Papillary breast cancers are usually small and are estrogen and/or progesterone receptor positive and HER2 receptor negative. The prognosis of this subtype is better than other invasive types. Papillary ductal carcinoma is usually treated with surgery, which may require additional therapy such as radiation, hormonal therapy, or chemotherapy.
Tubular ductal carcinoma accounts for less than 2% of breast cancers and usually occurs in women over 50 years of age. The cells of this carcinoma form tubular structures. Such tumors are usually positive for estrogen and/or progesterone receptors and negative for the HER2 receptor. The 10-year survival rate is 90-100%. Treatment often includes surgery as well as additional therapy such as radiation, hormonal therapy, or chemotherapy.
Lobular carcinoma. It comes from the milk lobules (glands that produce breast milk).
Non-invasive lobular carcinoma originates in the milk lobules and usually does not spread through the wall of the lobules to the surrounding tissue of the breast or other parts of the body. It is less common and, apparently, also begins in the ducts *. Although it is a non-invasive tumor, its presence signals an increased risk of developing invasive cancer later (about 25%), and can appear in any part of the breast – both in the lobules and in the ducts. Due to the non-aggressive nature of the tumor, the doctor may order observation with more frequent examinations for early diagnosis of possible invasive cancer.
Invasive lobular carcinoma begins in the milk lobules, then invades (invades) adjacent tissue, and can spread (metastasize) to distant parts of the body. This type of breast cancer accounts for 10% of invasive breast cancer cases. The 10-year survival rate is 35-50%. Treatment options for invasive lobular carcinoma depend on the extent of the lesion, and include localized approaches (such as surgery and radiation therapy) that treat the local tumor and surrounding areas, and systemic therapies (such as chemotherapy and hormonal or targeted therapies) that work throughout the body to kill cancer cells that may have spread from the original tumor.
Other types.
Inflammatory Breast Cancer (IBC) is a rare type of breast cancer that causes blockage of the lymphatic vessels in the breast skin. The term «inflammatory» is not associated with inflammation per se, but with the appearance of itchy, red, sensitive, warm and hard breasts as a result of the accumulation of leukocytes and stimulation of blood flow in the skin. This type of cancer differs from other types mainly in terms of symptoms, prognosis, and treatment.
Because of the similarity of symptoms, inflammatory cancer can be misdiagnosed as a breast infection such as mastitis. If a doctor prescribes antibiotics, but the symptoms do not disappear within seven to ten days, then this may be a sign of inflammatory cancer. The danger of this cancer is that it can grow rapidly and aggressively, and is usually diagnosed already at an advanced stage - IIIB or IV. Treatment for inflammatory breast cancer usually includes chemotherapy followed by surgery (up to complete removal of the breast) and radiation therapy. Additionally, hormonal and/or chemotherapy may be involved.
Paget's disease is a cancer of the nipple, in the initial stage of which eczema-like skin lesions appear on the nipple and areola, and the nipple itself increases in volume, thickens and swells. In this case, the tumor itself is sometimes hidden inside the breast tissue. This type of breast cancer occurs in less than 3% of breast cancer cases. About half of the cells are positive for estrogen and progesterone receptors, and most of them are positive for HER2. The primary treatment for Paget's cancer is most often surgical removal of the tumor. Early detection allows sparing surgery, while late stages may require removal of the entire breast.
Other rare types of breast cancer include breast sarcoma, metaplastic carcinoma, adenocystic carcinoma, phyllode tumor, and angiosarcoma.
Metastatic breast cancer, also known as stage IV or advanced breast cancer, is breast cancer that has spread to other organs in the body. Although more than 90% of breast cancer patients are diagnosed at an early stage of the disease, about 25% of them will eventually die from distant metastases. Even after the original tumor is removed, microscopic tumor growths may remain in the body, allowing the cancer to return and spread. Metastases from breast cancer are usually found in the lymph nodes in the armpit, around the collarbone and sternum; but they can be transferred to any part of the body. Most often, breast metastases affect organs such as the lungs, liver, bone and brain.
Patients may be diagnosed with metastatic disease initially, or metastases may develop months or years after treatment of the primary tumor. The risk of breast cancer returning and metastasizing varies from person to person and is highly dependent on the biology of the tumor and the stage of the disease at the time of initial diagnosis. Treatment of metastatic breast cancer includes all the same methods of treatment as other stages of breast cancer: surgery, radiation, targeted, hormonal and chemotherapy.
Staging assesses the extent to which the cancer has progressed and is determined by the size of the tumor and by whether it has spread to the lymph nodes or other parts of the body.
The TNMG notation helps to describe the extent of the disease in more detail.
The T value estimates the size of the tumor; N - spread to lymph nodes; and M is tumor metastasis. An additional indicator G assesses the degree of cell differentiation, which affects the prognosis of the disease.
T - primary tumor
Tx - insufficient data to evaluate the primary tumor;
T0 - the primary tumor is not determined;
Tis – carcinoma in situ (non-invasive);
Tis (DCIS) - carcinoma in situ in ducts;
Tis (LCIS) - carcinoma in situ in lobules;
Tis (Paget's) - Paget's cancer without a sign of a tumor;
T1 - tumor up to 2 cm in greatest dimension;
T2 - tumor up to 5 cm in greatest dimension;
T3 - tumor more than 5 cm in greatest dimension;
T4 - Tumor of any size with direct extension to the chest wall or skin.
N - local lymph nodes
Nx - insufficient data to assess the state of local lymph nodes;
N0 - no signs of metastatic lesions of local lymph nodes;
N1 - metastases in the mobile axillary nodes on the side of the lesion;
N2 - metastases in the axillary lymph nodes from the side of the lesion, fixed between themselves or with surrounding structures;
N3 - metastases in the lymph node from the side of the lesion with/without damage to the axillary lymph nodes or metastases with damage to the lymph nodes.
M - distant metastases
Mx - insufficient data to determine distant metastases;
M0 - distant metastases are not determined;
M1 - distant metastases are determined.
G - histopathological gradation
Gx - the degree of differentiation cannot be determined;
G1 - high degree of differentiation;
G2 - average degree of differentiation;
G3 - low degree of differentiation;
G4 - undifferentiated tumor.
Stage 0: non-invasive (in situ) ductal carcinoma; the tumor cells are confined within the milk duct and there is no evidence that they invade the surrounding tissues.
This is the earliest stage of breast cancer and is sometimes considered a precancerous condition. It is generally accepted that ductal carcinoma in situ is safe because the tumor does not metastasize and spreads to healthy breast tissue. However, not all experts agree with this. Many types of breast cancer at this stage do not need antitumor treatment, but require careful monitoring, as they can easily degenerate into aggressive cancer either on their own or as a result of treatment.
The results of therapy are usually very successful. The five-year survival rate for stage 0 breast cancer is 93%.
The problem here is that breast cancer at this stage is difficult to detect and patients may not be aware of it. The seal in the problem area may not be palpable, and other symptoms may be absent. However, a lump may be detected through annual screening, during a breast biopsy, or by chance for some other reason, although more often than not, a lump found will not be associated with a tumor.
Stage I: at the beginning of this stage, the tumor does not extend beyond the breast, does not exceed 2 cm across, and does not affect any lymph nodes.
Stage I breast cancer is the initial stage of invasive breast cancer. At this stage, the cancer cells have already spread beyond their original location into the surrounding breast tissue. Because the stage I tumor is small, it can easily be overlooked. However, regular breast self-examinations by palpation and annual screening are very important as they can lead to early diagnosis of a tumor. The risk of metastasis is low *.
Stage I is divided into two categories:
• IA: Tumor size does not exceed 2 cm (pea or hazelnut size) and does not extend beyond the breast.
• IB: Small clusters of cancer cells (up to 2 mm in size) are found in the lymph nodes, and the tumor is either absent or less than 2 cm across. The survival rate for stage IA may be slightly higher than for stage IB. However, the prognosis for all patients with stage I breast cancer is considered good.
Most often, stage I breast cancer looks like:
• T: T1, T2, T3, or T4, depending on the size and/or grade of the primary tumor.
• N0: The cancer has not spread to the lymph nodes.
• M0: The disease has not spread to other parts of the body.
Stage II: the tumor is larger than 2 cm across and has begun to spread to nearby lymph nodes.
Stage II breast cancer indicates a slightly more advanced form of breast cancer. Although at this stage the cancer is still not found in distant parts of the body, the risk of metastasis remains high. At stage II, the tumor can be detected during self-examination of the breast in the form of a compacted formation in the breast.
Stage II is divided into two categories:
• IIA: One of the following statements is true:
- there is no tumor in the breast, but the cancerous lesion has spread to the axillary lymph nodes; or
- the size of the tumor in the breast is 2 cm or less, and the cancerous lesion has spread to the axillary lymph nodes; or
- the size of the tumor in the breast is 2-5 cm, but the cancerous lesion has not spread to the axillary lymph nodes.
• IIB: One of the following statements is true:
- the size of the tumor is 2-5 cm, and the cancerous lesion has spread to the axillary lymph nodes; or
- the size of the tumor is greater than 5 cm, but the cancerous lesion has not spread to the axillary lymph nodes.
The survival rate for stage IIA breast cancer may be slightly higher than for stage IIB. Sparing surgical removal of the tumor and affected lymph nodes in many cases allows you to save the breast, although the prognosis is somewhat worse. However, the prognosis for stage II breast cancer is considered favorable.
Most commonly, TNM describes stage II breast cancer as:
• T: T1, T2, T3, or T4, depending on the size and/or grade of the primary tumor.
• N1: The cancer has spread to the lymph nodes.
• M0: The disease has not spread to other parts of the body.
Stage III: the tumor is larger than 5 cm across, has spread extensively to nearby axillary nodes, and may spread to other lymph nodes near the chest. The risk of metastasis is very high.
Stage III breast cancer is a more advanced form of invasive breast cancer. At this stage, cancer cells are not usually found in more distant areas of the body, but they are present in several axillary lymph nodes. At this stage, the tumor can be quite large, and may have spread to the chest wall or to the skin of the breast.
Stage III breast cancer is divided into three categories:
• IIIA: One of the following statements is true:
- the tumor is not found in the breast, but the cancerous lesion has spread to the axillary lymph nodes that are attached to each other or to other structures, or it may be found in the lymph nodes near the breastbone; or
- the tumor is 2 cm or less; the cancerous lesion has spread to axillary lymph nodes that are attached to each other or to other structures, or it may have spread to lymph nodes near the breastbone or
- tumor size 2-4 cm; the cancerous lesion has spread to axillary lymph nodes that are attached to each other or to other structures, or it may have spread to lymph nodes near the breastbone or
- the tumor is more than 5 cm; the cancerous lesion has spread to the axillary lymph nodes, which may be attached to each other or to other structures, or it may have spread to lymph nodes near the breastbone.
• IIIB: the tumor can be of any size, and the cancerous lesion:
- has spread to the chest wall and/or skin of the breast, and
- may spread to axillary lymph nodes, which may be attached to each other or to other structures, or it may spread to lymph nodes near the breastbone;
- has spread to the skin of the breast (inflammatory breast cancer).
• IIIC: One of the following statements is true:
- there may be no evidence of cancer in the breast, or the tumor may be of any size and may have spread to the chest wall and/or the skin of the breast;
- cancer cells are present in the lymph nodes above or below the collarbone;
- cancer cells may have spread to the axillary lymph nodes or lymph nodes near the breastbone.
- the cancer has spread to the skin of the breast (inflammatory breast cancer).
Breast cancer stage IIIC can be resectable or inoperable:
- resectable stage IIIC: the cancerous lesion is in 10 or more axillary lymph nodes or is in the lymph nodes below the collarbone, or is in the axillary lymph nodes and lymph nodes near the breastbone;
- inoperable stage IIIC: the cancerous lesion has spread to the lymph nodes above the collarbone.
The breast cancer survival rate for stage IIIA may be slightly higher than for stage IIIB, and the survival rate for stage IIIB may be slightly higher than for stage IIIC. However, in all patients with stage III breast cancer, there are several promising treatment options.
Higher TNM scores indicate more extensive disease. Most commonly, stage III breast cancer is described as:
• T: T1, T2, T3, or T4, depending on the size and/or grade of the primary tumor.
• N1: The cancer has spread to the lymph nodes.
• M0: The disease has not spread to other parts of the body.
Stage IV: the tumor has spread to distant organs, such as the bones, liver, brain, or lungs.
Stage IV breast cancer is also called terminal cancer. Here, the cancerous lesion has spread elsewhere in the body; most often it is the bones, brain, lungs or liver, while several organs can be affected at the same time.
Despite the variety of treatment options, the prognosis for this stage is poor.
Higher TNM scores indicate more extensive disease. Most commonly, stage IV breast cancer is described as:
• T: T1, T2, T3, or T4, depending on the size and/or grade of the primary tumor.
• N1: The cancer has spread to the lymph nodes.
• M1: The disease has spread to other parts of the body.
Recurrence: the disease returned after previous treatment.
Most cancer recurrences appear within the first two to three years after treatment. In the absence of recurrence within 5 years, the disease is considered cured. However, breast cancer can recur even 25 years later *, although it will be considered a new cancer. Breast cancer can recur in the breast, chest, or elsewhere in the body.

Breast cancer that returns to its original location (the area where the operation was performed) is called a local recurrence. A recurrence in another part of the body is called metastatic breast cancer, or regional recurrence. Cancer cells can migrate from the original tumor in the breast to other parts of the body via the lymphatic system or the bloodstream. Even when a metastatic breast tumor spreads to another part of the body, it contains the same cancer cells that previously developed in the primary tumor. These cells can remain dormant for many years until they again begin to form a secondary tumor.
In order to detect recurrence as early as possible, it is important to constantly monitor your health, regularly screen and monitor key indicators, and inform your doctor about possible signs of breast cancer recurrence.
Signs and symptoms of local recurrence of local recurrence of breast cancer are the same as those of the original cancer and may include:
• an increase in the size or shape of the breast;
• lesions or knots felt on or inside the breast;
• skin changes such as swelling, redness or other visible differences;
• inflammation or area of redness on the skin of the breast;
• papillary secretions other than breast milk;
• irritated or itchy breasts.
Signs and symptoms of metastatic breast cancer may include:
• changes or lumps in the lymph nodes;
• unexplained pain in other areas of the body, such as bones;
• difficulty breathing or persistent cough;
• loss of appetite and/or weight loss;
• severe headaches.
Women with early breast cancer are most likely to develop local recurrence within the first five years after treatment. On average, during this time, 7-11% of women with early breast cancer experience a local recurrence. For patients with a family history of cancer or a BRCA1 or BRCA2 gene mutation, both the risk of breast cancer and the rate of cancer recurrence are higher. The risk of finding new cancers, such as ovarian cancer, may also be higher, especially with hormone therapy. The risk of cancer recurrence is based on many factors, including the type of cancer and prior therapy.
The prognosis of the
The stage of development of the disease is the main prognostic factor. The lower the stage, the lower the risk of relapse (return of the disease) and the higher the patient's survival.
Lymph node involvement is the second most important prognostic factor. The spread of cancer cells to the lymph nodes increases the risk of recurrence and reduces the favorable prognosis. The greater the number of affected lymph nodes, the higher the risk of further development of breast cancer. The highest risk of recurrence is when cancer cells spread to four or more lymph nodes.
Degree of differentiation. Tumors with highly differentiated cells have a better prognosis because they grow more slowly and are less aggressive than tumors with poorly differentiated cells.
Hormone receptor status. In general, the greater the variety of sensitive hormone receptors the cells have, the more favorable the prognosis. Hormone-positive tumors are usually more differentiated, less aggressive, less prone to metastasis, and more amenable to therapy than hormone-negative ones.
Age at the time of diagnosis. Although the overall risk of disease increases with age, younger women (under 35) have more aggressive tumors, are often diagnosed at more advanced stages, and have a higher risk of recurrence. Thus, younger women have a worse overall prognosis than older postmenopausal women.
Recurrence prognosis. The following factors may affect the prognosis of breast cancer that has returned after previous treatment.
The period between treatment and relapse. The longer the period from the end of therapy to tumor recurrence, the more favorable the prognosis. Women whose breast cancer returns more than 5 years after diagnosis usually have a better outcome than women who relapse less than 2 years after diagnosis.
Place of recurrence. Even if a secondary tumor has formed in another organ within 5 years, it will be considered metastatic breast cancer.
A tumor that reappears in the mammary gland after surgical and radiation therapy (local recurrence) has a more favorable prognosis than a tumor that has appeared in other organs (remote recurrence or distant metastases).
Relapses in the pectoral muscles are associated with a high probability of the formation of a distant relapse, which worsens the long-term prognosis.
Relapses in the liver, lungs, or brain have a worse prognosis than relapses in other parts of the breast, chest muscles, and axillary lymph nodes.
Bone relapses have a better prognosis than liver, lung, or brain relapses, but worse than breast or chest muscle relapses.
But, despite all these relapse factors, you should never give up and rely on fate. We need to learn and act. Treat and believe in success. The road will be mastered by the walking one.